HuBMAP | VU TMC Eye/Pancreas | Histopathology Assessment of Human Pancreas
Alvin C. Powers, Adel Eskaros, Jordan Wright, Annika Windon
Abstract
The purpose of this protocol is to outline the parameters for pathologic and morphologic assessment of human pancreatic tissue. This protocol was developed for tissue specimens prepared via formalin fixation and paraffin embedding by the HuBMAP Tissue Mapping Center at Vanderbilt. It provides a rapid but comprehensive initial assessment, though it should not be considered a substitution for formal pathology analysis. For assessment of gross morphology, please see HuBMAP | VU TMC Eye/Pancreas | Human Pancreas Processing for Multiple Applications.
Steps
Image H&E-stained tissues prepared according to standard protocol using a whole-slide digital scanner (Aperio ScanScope or Zeiss AxioScan) at 20X magnification. Slides may also be reviewed under a light microscope (Olympus Bx41).
Download example H&E images (shown in Figures here): Pancreas Histopathology Assessment_H&E.pdf
Assess and record pathologic and morphologic features using the attached template, reviewing at least one block from each anatomical region of the organ (head, body, and tail). Features listed in the template are described in detail in the following steps. Features listed in the template are described in detail in the following steps. Sub-steps detail further assessment to confirm and/or supplement initial pathology review.
Evaluate the endocrine pancreas:
Islet number: normal, reduced, or increased?
Islet size: normal (i.e., a range of sizes), smaller, or hypertrophied?
Islet shape: normal (compact; oval/rounded and well demarcated) or diffuse (irregular)?
Amyloidosis: yes or no?
- If yes, specify % of islets affected.
Islet fibrosis: yes or no?
- If yes, specify % of islets affected.
Islet hydropic degeneration: yes or no?
- If yes, specify % of islets affected
Islet inflammation: yes or no?
- If yes, specify intraislet or peri-islet and number of islets affected.
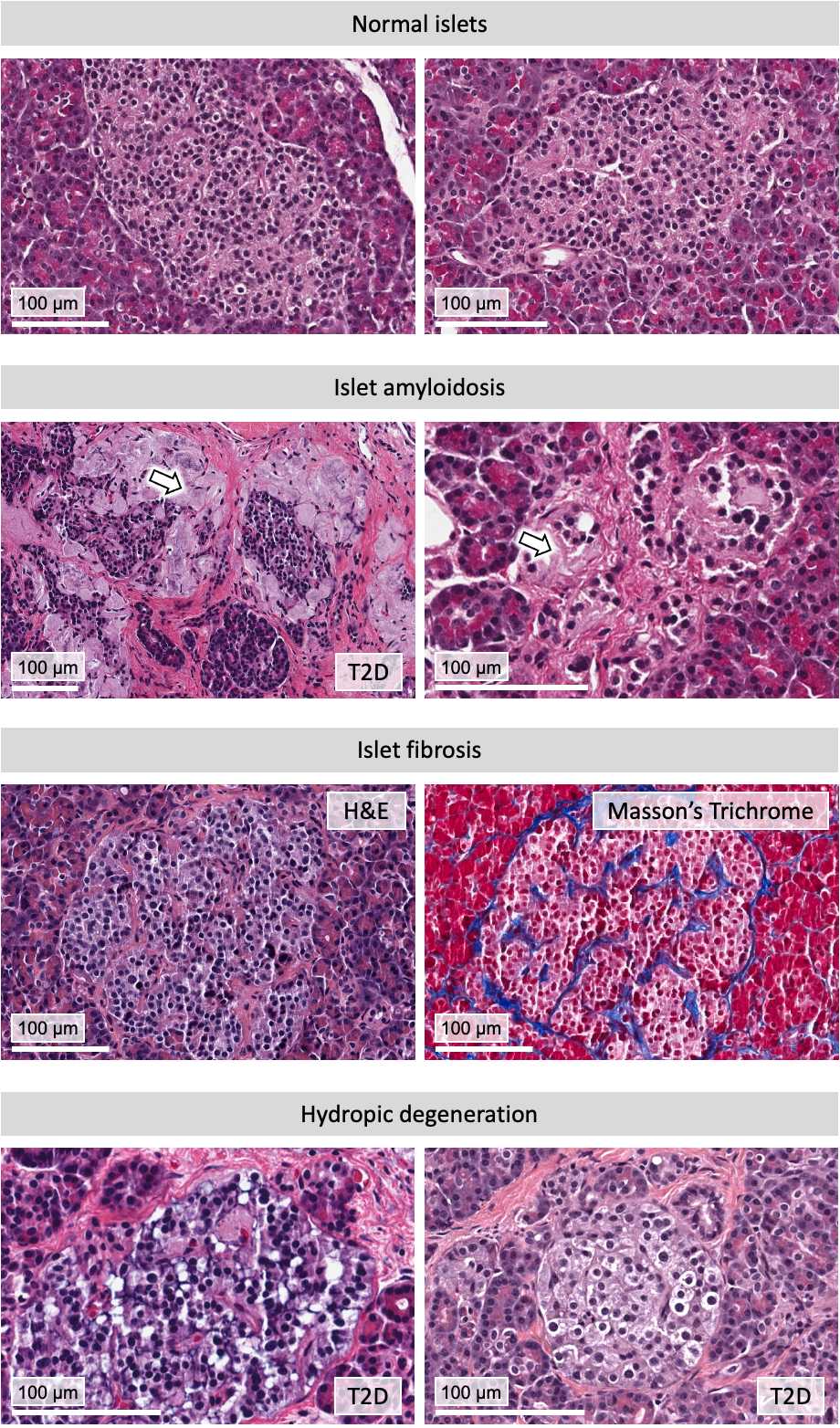
Use Congo red stain to confirm/differentiate with islet hyaline fibrosis; expect amyloidosis in diabetic and prediabetic individuals (consider A1C and BMI) and in old age.
Evaluate the exocrine pancreas:
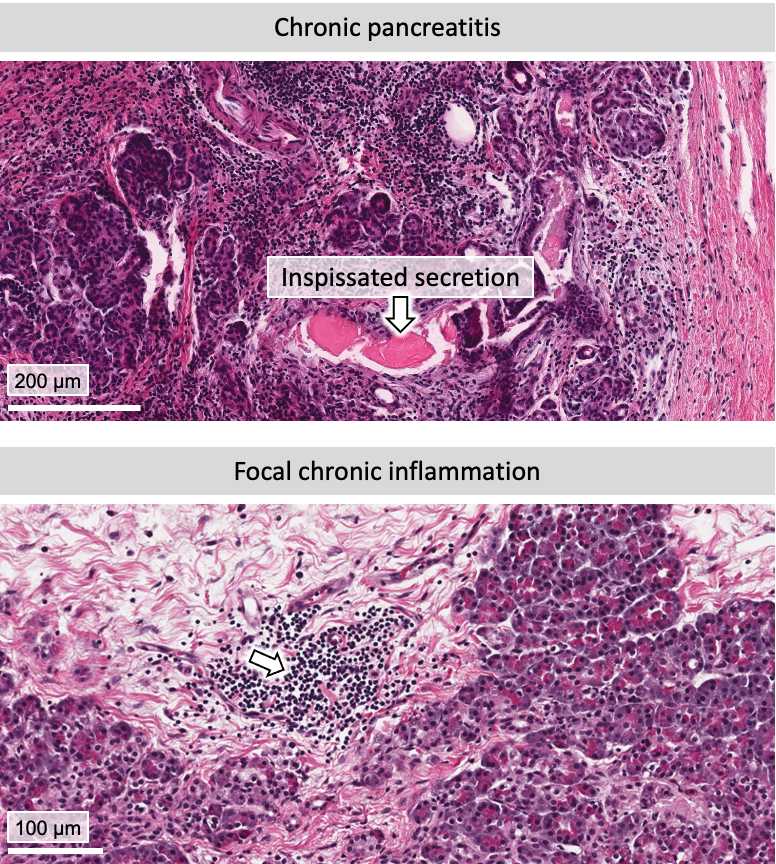
Evidence of pancreatitis: yes or no?
- If yes, specify: acute or chronic?
- If yes, specify: focal (one lobe) or diffuse (multiple lobes)?
- If yes, specify severity (mild, moderate, or marked)
▷ Acute: It can be mild interstitial pancreatitis with oedema and acute inflammatory cells but no necrosis, or necrotizing with acute inflammation and pancreatic necrosis. Refer to: Lankisch et al., 2015.
▷ Chronic: Cardinal features include fibrosis, acinar atrophy, ductal change, chronic inflammatory cells (histology is not the gold standard; it needs clinical and laboratory data for diagnosis). Refer to: Esposito et al., 2020 and Korpela et al., 2022.
Autolysis: yes or no?
- If yes, specify partial or complete
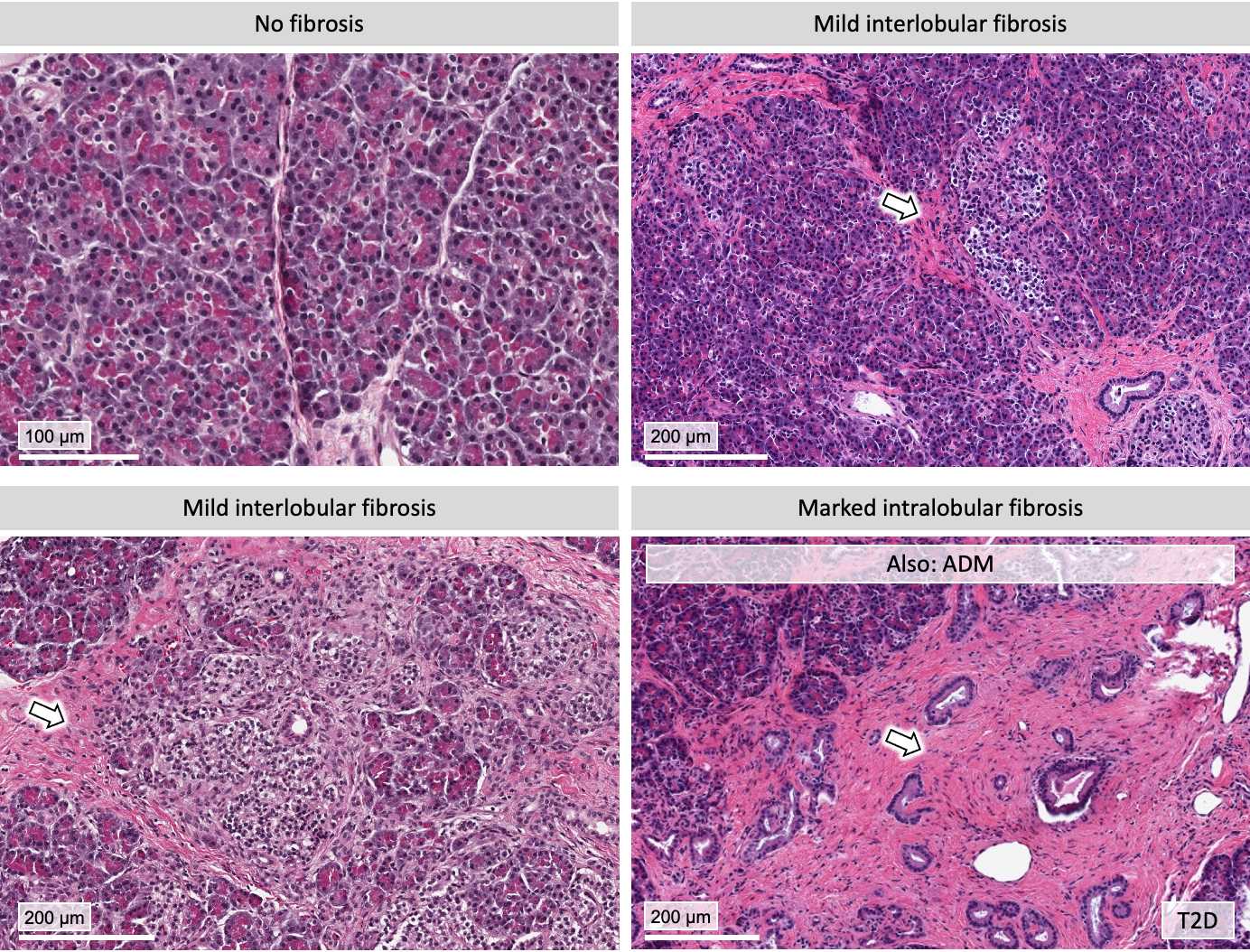
Fibrosis: yes or no?
- If yes, specify intralobular, interlobular, or periductal/perivascular
- Specify severity (mild, moderate, or marked)
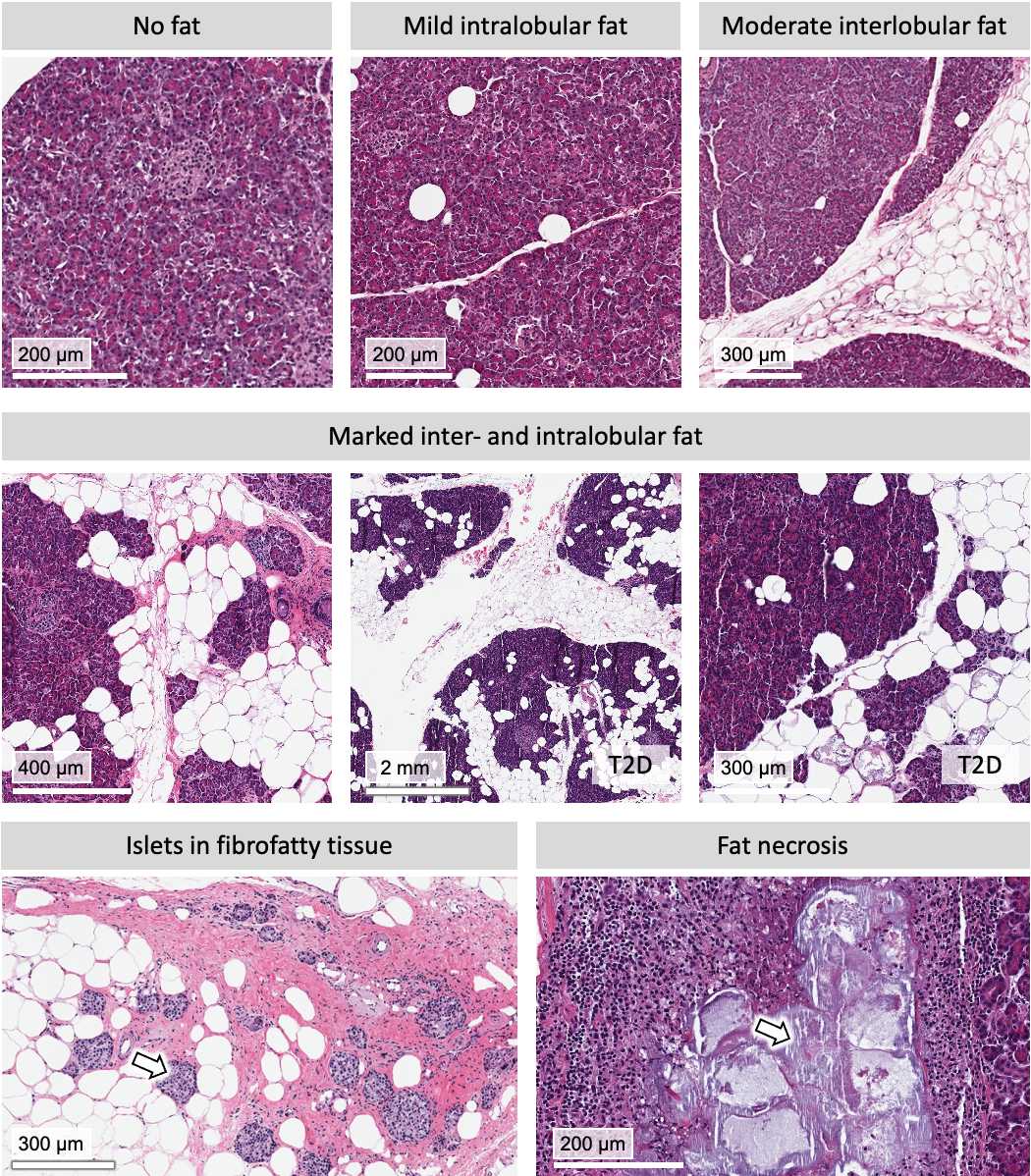
Fat infiltration: yes or no?
- If yes, specify intralobular or interlobular
- Specify severity (mild, moderate, or marked)
Fat necrosis: yes or no?
- If yes, specify % of tissue area
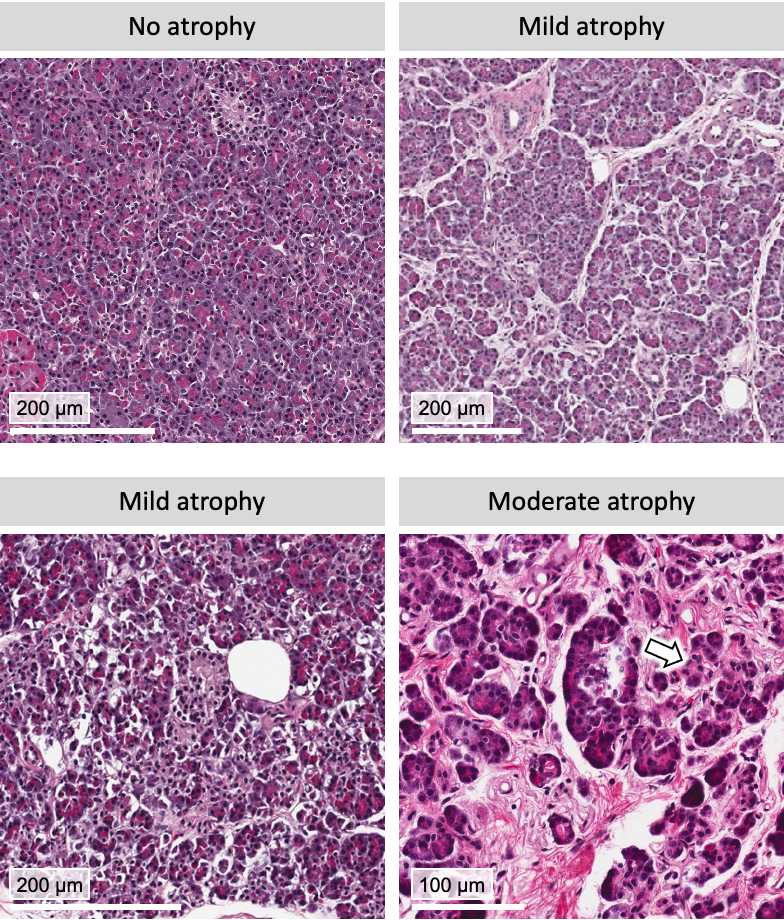
Acinar atrophy: yes or no? [see description below]
- If yes, specify severity (mild, moderate, or marked)
▷ Acinar atropy is defined as destruction of acinar tissue with fibrosis replacement, acini smaller in size with fewer number of cells.
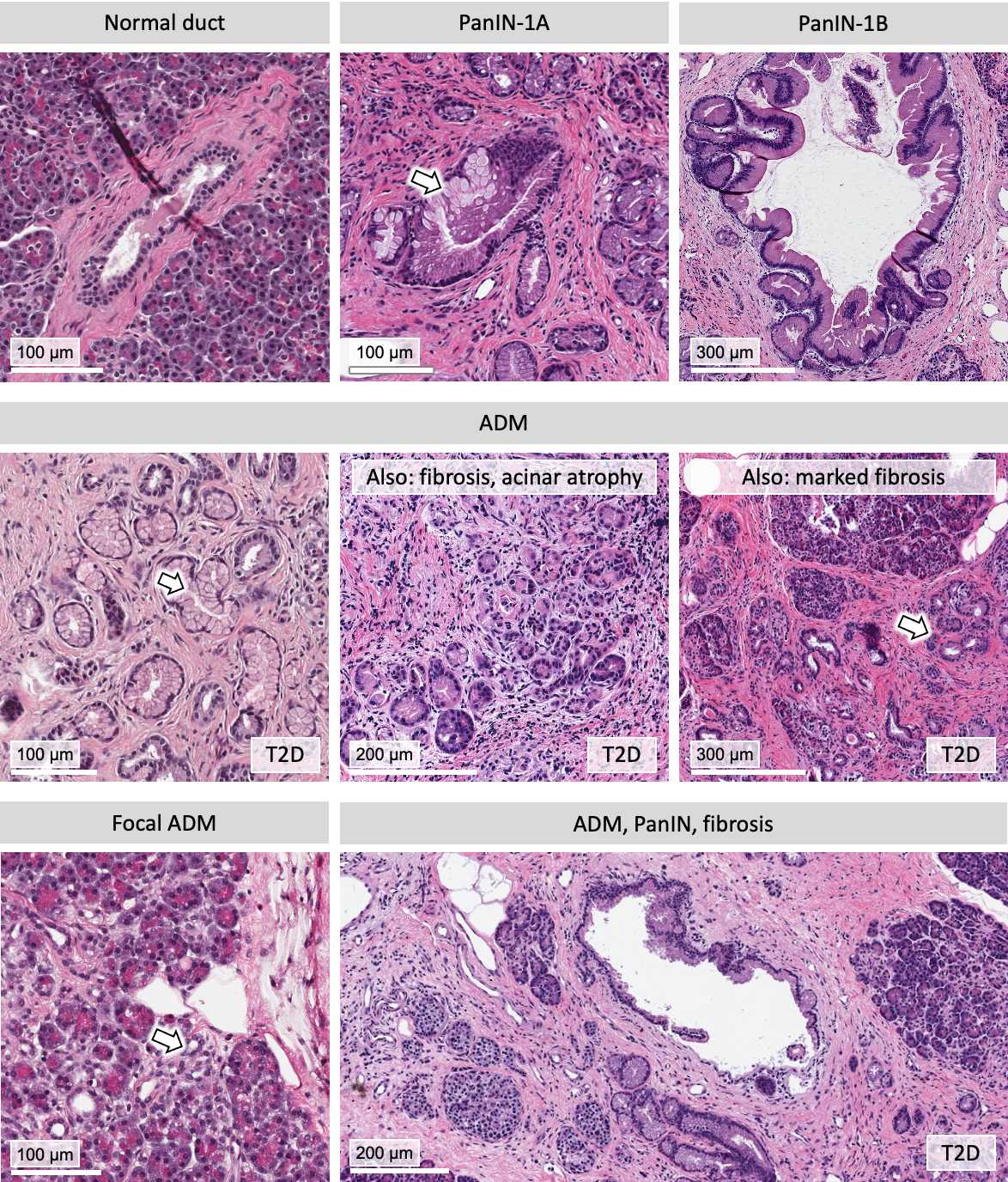
Duct system: normal or abnormal?
- If abnormal, is there dilation?
- If abnormal, is there obstruction?
- If yes, what is the cause? (inspissated secretion/stone)
Neoplasia: yes or no?
- If acinar to ductal metaplasia (ADM), specify number of lobules/lesions and whether it is focal
- If pancreatic intraepithelial neoplasia (PanIN), specify the grade (1A, 1B, 2, or 3)
- If other neoplasia, describe
▷ ADM: transformation of acinar cells to duct-like morphology; may progress to pyloric metaplasia (with mucus production) or to PanIN.
▷ PanIN: ductal structures with enlarged lumen; may show papillae or dysplastic changes; may end with cancer formation (PDAC).
▷ Other: includes squamous metaplasia, intraductal papillary mucinous neoplasm (IPMN), and mucinous cystic neoplasm (MCN).
Refer to: Li and Shu, 2022.
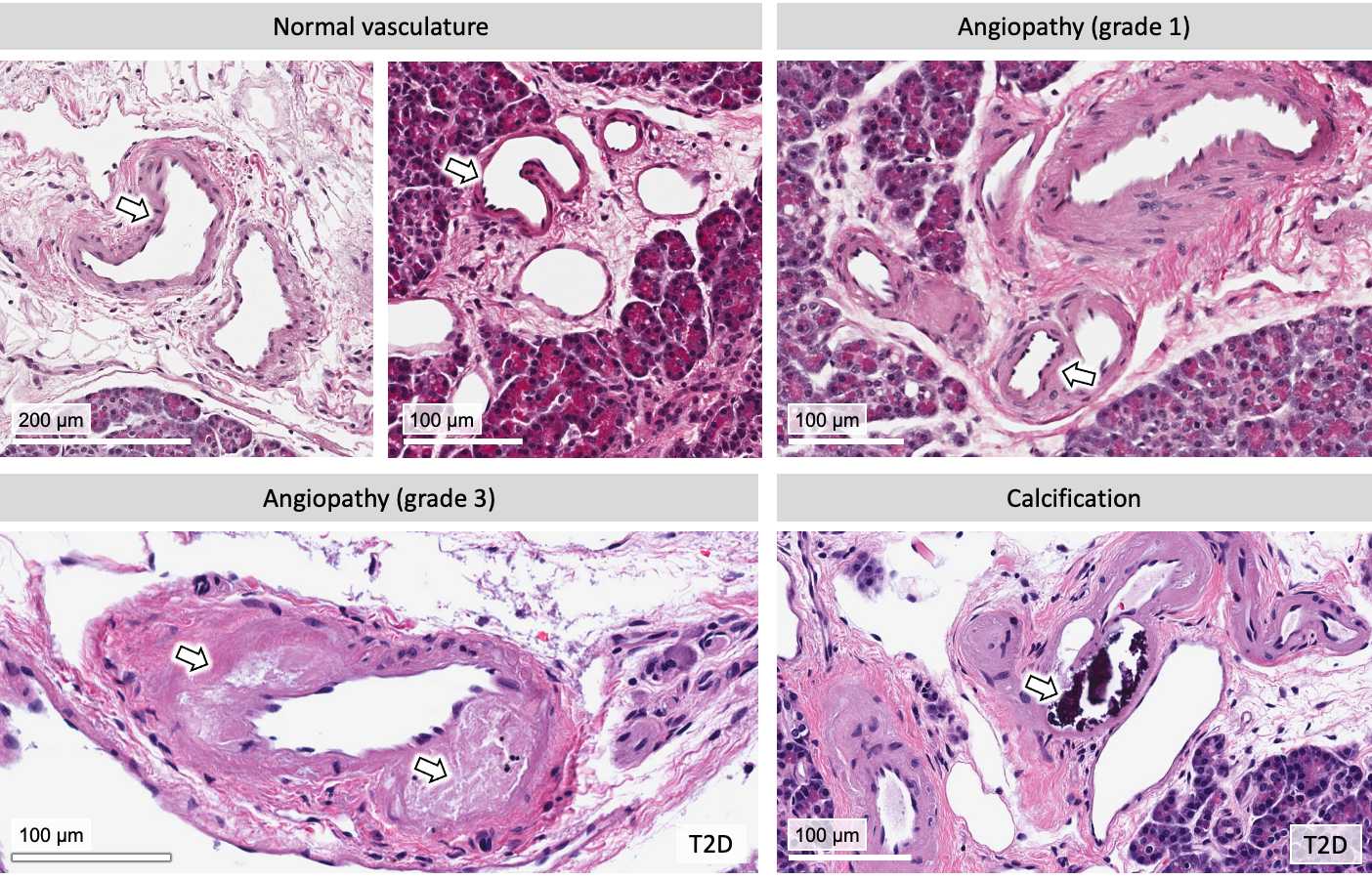
Evaluate the vasculature:
Angiopathy: normal or abnormal?
- If abnormal, is there evidence of calcification?
- If abnormal, is there arteriosclerosis/arteriolosclerosis?
- If yes, give grade (0-4)
Refer to: Ling et al., 2020.
Provide any additional comments as needed.

